Stay ahead of the curve as a political insider with deep policy analysis, daily briefings and policy-shaping tools.
Request a DemoOPINION: How Georgia can better support children and families amid Medicaid unwinding

(Credit: Kabita Darlami)
By Laura Colbert, Callan Wells and Brittany Newton
Since last April, we have answered phone calls, emails, and texts from frustrated Georgia families struggling through their Medicaid renewals. In one such exchange, “Naomi” shared that her 4-year-old grandson's Medicaid coverage was canceled without any notice. They found out hours before her grandson’s regular dentist visit and a doctor’s appointment for school-required vaccines.
Naomi — a savvy woman with a professional degree and previous high-level executive positions — could not get in touch with a state employee about restarting her grandson’s coverage. After calling and being placed on hold for more than two hours over several calls, she tried to visit the local county Medicaid office only to find it closed.
Naomi was never able to speak with one of Georgia’s customer service agents, who are supposed to be available to help with questions like these. Instead, she worked through professional connections (an asset that many families don’t have) to restore her grandson’s coverage after two months of delay.
Georgia is 10 months into the year-long “Medicaid unwinding” in which the state is required to assess almost every Medicaid member to determine if they are eligible to keep their health coverage. Most of Georgia’s 2.8 million Medicaid members are children. The program also covers low-income people with disabilities, seniors, pregnant women, new mothers (until their child’s 1st birthday), and a few other very limited groups.
So far, more than 500,000 Georgians have lost their Medicaid coverage. Only 73,300 (14%) have lost coverage because the state knows they are no longer eligible. The remainder were disenrolled simply because the state is missing information, can’t get in touch, or documents go missing. In June 2023, some 7 out of 10 Georgians who lost Medicaid were children. Because the state hasn’t released child-specific data for any month since, we can’t tell how many total kids have become uninsured.
With only a few months left in Georgia’s Medicaid unwinding, we know that this process has been frustrating and consequential for families. At a recent event in DeKalb County, more than 400 families showed up so they could get help with their Medicaid eligibility determinations because they’ve struggled on their own.
Many families across the state haven’t had the benefit of in-person assistance. Some are temporarily uninsured, and others will go without health coverage for years.
Georgia has struggled more than most states to carry out the unwinding process, but none of the pain points should be surprising.
For years, it has been challenging for Georgians to enroll in, renew, and keep their public benefits (Medicaid, SNAP food assistance, etc.). The systems that families must navigate often seem purposefully difficult, and even hostile to the people they are meant to help.
As Naomi’s story illustrates, the Medicaid renewal process begins with a printed and emailed notice to let the member know that their coverage is due for renewal and what actions they need to take. These notices regularly fail to reach members, and when they do, the notices are hard to understand without a law degree, or they convey conflicting information.
When Medicaid members look for help, they report being unable to reach anyone through the state’s call line. Their county public benefits office may only be open one to three days per week for a narrow part of the work day. Sometimes when families are able to find the help they need and submit required paperwork, there is no guarantee that they will get or keep Medicaid because of computer system errors.
Even systems meant to streamline renewals and applications haven’t yet helped many Georgians. Only 35% of Georgia’s Medicaid members whose renewals are complete have been renewed automatically by the state. All other renewals have taken some kind of manual work by the member or their family and state workers.
State lawmakers approved an “express lane” option in 2022, which allows children applying for food assistance to also be considered for Medicaid with just one application. During the unwinding, assistants helping Georgians with their Medicaid and food assistance renewals noticed that kids were not automatically being considered for these programs without the family’s active permission for each child. An “express lane” should be the default option for kids — especially when we remember that food and health care can be difference makers for families living paycheck-to-paycheck. To Georgia’s credit, the state is changing this feature to be automatic for children after hearing this feedback.
If Georgia were to follow our leaders’ oft-repeated mantra to run our state more like a business, we would have overhauled our public systems and policies years ago to be convenient, easy to use and dignified.
The state should prioritize paying knowledgeable state workers fairly for their expertise as they process benefits applications and help families with questions. Case workers currently make an average of $35,000 annually which has contributed to poor morale and high turnover rates. A pay raise would improve the retention of workers and help ensure families can reach someone when they call or try to find in-person help before or after their work shifts.
Georgia’s Technology Authority should do a full review of the Gateway public benefits system to identify opportunities to update and improve this technology. Built and managed by Deloitte, the system is expensive, clunky, and takes months to update when problems are identified. It can also be hard to use on mobile devices, which is many families’ only access point.
Any updates and improvements should begin with leaders asking the families who use our state’s public systems for their feedback and input. They are the experts in what does and doesn’t work because they are navigating all of it. They will expertly describe outcomes that will work better for their family and which would likely include ideas like using easier language in printed and digital materials; re-locating public benefits workers to libraries or recreation centers where families are already spending time; or creating a user-friendly app that allows them to easily upload pictures of requested documents or check the status of their application.
We could also reduce the opportunities that currently exist for kids (and their parents) to lose their health coverage. Georgia could follow in the footsteps of seven other states that guarantee that Medicaid-eligible babies leave the hospital with coverage and keep it through their sixth birthday, with no renewals or interruptions. Not only would this help kids and families, it would also relieve state workers so they can focus on applications and renewals for other Georgians.
Insured parents are more likely to have healthy, insured children. So let’s make it easier for parents too by raising the Medicaid income limits for parents. Right now, parents have to either make less than $7,800 per year for a family of four or meet the most stringent work requirements in the country to qualify for coverage. Our state leaders have the power to change that so that $31,200 for the same family qualifies parents for coverage.
The Medicaid unwinding has been a challenge for all states, but it didn’t have to be this hard on Georgia families. Let’s avoid this kind of upheaval in the future by making changes now. Our state leaders are in the midst of decisions about how to spend our tax dollars this year and what changes state agencies will need to make as they serve Georgia families. These improvements should go to the top of their lists.
Laura Colbert is executive director of Georgians for a Healthy Future, Callan Wells is senior health policy manager for Georgia Early Education Alliance for Ready Students, and Brittney Newton is senior policy analyst for Voices for Georgia’s Children.
Read this story for free.
Create AccountRead this story for free
By submitting your information, you agree to the Terms of Service and acknowledge our Privacy Policy.
House speaker Jon Burns hires new communications director
House speaker Jon Burns, R-Newington, announced today that he has hired a new communications director. Kayla Roberson, who has served as press secretary at the Georgia Chamber for the past year or so, will now oversee all external communications, media relations and strategic messaging for Burns.
“I’m excited to welcome Kayla to our team,” Burns said in a statement. “Kayla has an excellent background, deep skill set and strong work ethic, and we’re excited to have her on board to continue getting our message out and sharing the House’s priorities ahead of and into the next session.”
A double major in political science and journalism at the University of Georgia, where she graduated in 2022, Roberson interned for U.S. Rep. Andrew Clyde, a Republican in north Georgia’s 9th Congressional District, and worked as a consultant for GOP political candidates before joining the Georgia Chamber.
“I’m beyond grateful for the opportunity to work under the leadership of speaker Burns,” Roberson told State Affairs. “Whether it’s improving education opportunities, putting money back in the pockets of hardworking Georgians, creating jobs or supporting our rural communities, speaker Burns always prioritizes doing what is best, and what is right, for Georgia.”
Political strategist Stephen Lawson, who has held the top communications role for the speaker since last December, announced he’s joining Dentons, where starting today he’ll lead the global law firm’s public affairs efforts.
Have questions or comments? Contact Jill Jordan Sieder on X @journalistajill or at [email protected].
Global bird flu disrupts Georgia exports, costing chicken producers millions
ATLANTA — A global bird flu that has rapidly spread from birds to dairy cows, milk supplies and humans has cost untold millions of dollars in lost export business in Georgia, the nation’s leading poultry producer, officials with the state Department of Agriculture and poultry industry said.
Georgia has had only three reported cases of H5N1 avian influenza since it reemerged in 2022. The last of those cases was resolved in November 2023 but ramifications of those outbreaks continue to have a big effect on the state’s ability to export chicken and chicken parts, such as chicken feet, to different countries, including China, one of Georgia’s biggest export markets for chicken feet.
In 2022, frozen chicken feet, for example, accounted for more than 85% of all U.S. poultry exported to China, according to Farm Progress, publisher of 22 farming and ranching magazines.
The $30 billion poultry industry is Georgia’s largest segment in its No. 1 industry — agriculture.
China has also placed a ban on the import of chicken products from 41 other American states. The ban on Georgia products went into effect Nov. 21, 2023. Efforts to reach the Chinese Embassy in Washington, D.C. were unsuccessful.
Georgia Poultry Federation President Mike Giles estimates the state’s loss at “well into the millions of dollars.”
“It’s a significant amount in a significant export market for us,” he said. “Poultry paws [feet] immediately lose value because of the loss of demand.”
The ban has forced Georgia poultry producers to find alternative markets for their products that would normally be headed to China.
“Some are sold domestically, some are frozen and stored, hopefully to find markets later on, and some go to other countries,” Giles said.
This isn’t the first time China has banned U.S.-produced poultry products due to a bird flu outbreak. The country instituted a ban in January 2015 which lasted until November 2019 — even though U.S. poultry products were deemed free of the disease by August 2017.
After that ban was lifted, China’s appetite for American-produced chicken products became voracious.
In 2022, U.S. producers shipped nearly $6 billion in poultry meat and related products (excluding eggs) to over 130 countries. China has emerged as the second largest destination for U.S. poultry exports, increasing from $10 million in 2019 to a record $1.1 billion in 2022, according to Southern Ag Today.
Chicken paws, for instance, are eaten in many Asian countries, including the Philippines, Thailand, Indonesia and Korea.They can also be found on Chinese dim sum menus throughout the U.S. and are also popular in Jamaica, Trinidad, Russia and Ukraine in everything from soups and curries to fried snacks.
Three Georgia counties have reported H5N1 outbreaks since 2022. The most recent case was late last year. Henry, Sumter and Toombs counties each reported one case of H5N1 bird flu. Those outbreaks are resolved, poultry and state agriculture officials say.
“When HPAI cases are found in any state, that state is given a designation that could lead to foreign countries halting trade on poultry products from that state,” Georgia Department of Agriculture spokesman Matthew Agvent told State Affairs.
Not since 2016 has the United States experienced such a fast-moving case of the H5N1 avian influenza. In the last two months, the virus has spread in parts of the United States from birds to dairy cows, some milk supplies and humans. Two people — a Texas dairy worker and a prison inmate in Colorado who was killing infected birds at a poultry farm — are reported to have caught the virus, according to news reports. The outbreak is the largest in recent history, impacting both domestic poultry and livestock as well as wild birds and some mammal species.
State officials are continuing to monitor the national outbreak and its impact on Georgia.

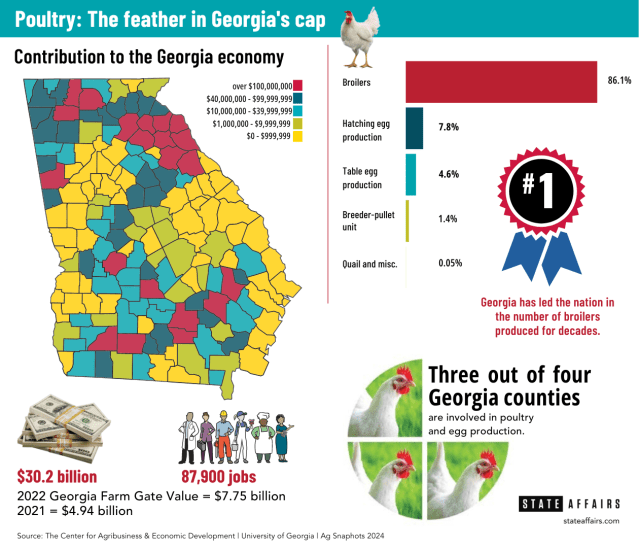
Georgia’s poultry & egg industry: At A Glance
Annual economic impact: $30.2 billion
Percentage of the Agriculture industry: 58% *
Jobs: 87,900
Counties involved in poultry & egg production: 3 out of 4
National ranking in chicken broiler production: No. 1
Daily production of table eggs: 7.8 million
Daily production of hatching eggs: 6.5 million
Pounds of chicken produced daily: 30.2 million
Pounds of chicken produced annually: 8 billion
Number of chicken broilers processed each day: 5 million
Counties involved in poultry & egg production: 3 out of 4
Source: Georgia Poultry Federation; The Center for Agribusiness & Economic Development, University of Georgia, Ag Snapshots 2024; Georgia Poultry Federation.
Have questions? Contact Tammy Joyner on X @lvjoyner or at [email protected].
Is it safe to eat chicken and eggs and drink milk? Answers to your most pressing questions about the latest bird flu outbreak
A two-year-old strain of bird flu has heightened concerns in Georgia and the rest of the country after the virus recently spread to dairy cows. Here’s what you need to know about the virus and its impact on Georgia and the rest of the country. What are the symptoms of this flu in humans? Eye …
Kemp signs bills on education, health care, taxes
Gov. Brian Kemp signed a slew of bills over the past week or so, including the private school voucher bill long sought by Republicans and a bill that will ease regulations over the construction and expansion of medical facilities in rural areas.
His bill-signing events were clustered into themes: education, health care, military members, human trafficking and Georgia’s coastal communities.
Education
Among the education-related bills Kemp signed was Senate Bill 233, also known as the Georgia Promise Scholarship Act, which provides the families of Georgia students enrolled in underperforming school districts with $6,500 scholarships that can be used toward private school or homeschooling expenses, including tuition, fees, textbooks and tutoring.
“Georgia is affording greater choice to families as to how and where they receive their education, while also continuing our efforts to strengthen public schools, support teachers, and secure our classrooms,” Kemp said, and thanked leadership in the House and Senate for prioritizing passage of the bill, which had failed in a close vote in 2023.
Democrats and many public education advocates who opposed the bill argued it will drain resources from public schools and primarily benefit students from wealthy families.
Kemp also signed Senate Bill 351, sponsored by nine Republican senators, which will require social media companies, as of July 1, 2025, to verify their users are at least 16 years old unless they receive approval from a parent.
House Bill 409, sponsored by Rep. Lauren Daniel, R-Locust Grove, directs school systems to consider not having bus stops where a student would have to cross a roadway with a speed limit of 40 mph or greater. The bill also increases the penalty for passing a stopped school bus to $1,000 from $250.
Kemp noted that Ashley Pierce, the mother of Addy Pierce, an 8-year-old who was fatally struck by a motorist as she boarded her school bus, “passionately advocated for and was instrumental in the passage of this legislation.”
Senate Bill 395, sponsored by Sen. Clint Dixon, R-Gwinnett, states that no school visitor or personnel can be prohibited from possessing an opioid reversal drug such as Narcan and directs schools to maintain a supply. It also allows opioid antagonists to be sold in vending machines and directs certain government buildings to maintain a supply of at least three doses.
Senate Bill 464, also sponsored by Dixon, creates the School Supplies for Teachers Program to financially and technically support teachers purchasing school supplies online. It also creates an executive committee of five voting members within the Georgia Council on Literacy and limits the number of approved literacy screeners to five, one of whom must be available to schools for free.
Health care
The governor chose his hometown of Athens as the venue to sign several bills aimed at improving health care in rural and underserved communities.
Among them was House Bill 1339, sponsored by Rep. Butch Parrish, R-Swainsboro, which revises the Certificate of Need process by which the state determines if and how new medical facilities can be built or expanded. The bill provides for several new exemptions, including psychiatric or substance abuse inpatient programs, basic perinatal services in rural counties, birthing centers and new general acute hospitals in rural counties. It also raises the total limit on tax credits for donations to rural hospital organizations to $100 million from $75 million.
Senate Bill 480, sponsored by Sen. Mike Hodges, R-Brunswick, establishes student loan repayments for mental health and substance use professionals serving underserved youth in the state or in unserved geographic areas disproportionately impacted by social determinants of health.
House Bill 872, sponsored by Rep. Lee Hawkins, R-Gainesville, chair of the House Health and Human Services Committee, expands cancelable loans for certain health care professionals to dental students who agree to practice in rural areas.
Senate Bill 293, sponsored by Sen. Ben Watson, R-Savannah, chair of the Senate Health and Human Services Committee, reorganizes county boards of public health and opens the qualifications for the CEO of each county board of health to include either licensed physicians or people with a master’s degree in public health or a related field.
Military members and veterans
Kemp on Wednesday focused on bills to improve military recruitment and provide more work opportunities for veterans and military family members.
House Bill 880, sponsored by Rep. Bethany Ballard, R-Warner Robins, allows spouses of military service members to work under a license they hold in good standing in another state while under the supervision of an existing Georgia medical facility or provider.
Senate Bill 449, sponsored by Sen. Larry Walker, allows military medical personnel to practice for 12 months while a license application is pending, including working as a certified nursing aide, certified emergency medical technician, paramedic or licensed practical nurse. The bill also creates a new advanced practice registered nurse license and makes it a misdemeanor to practice advanced nursing without a license.
Human trafficking
The governor on Wednesday was accompanied by first lady Marty Kemp and other members of the GRACE Commission for the signing of an anti-human trafficking package. It includes Senate Bill 370, which adds certain businesses to the list of organizations that must post human trafficking notices, including convenience stores, body art studios, businesses that employ licensed massage therapists and manufacturing facilities.
Sponsored by Sen. Mike Hodges, R-Brunswick, the bill also allows the Georgia Board of Massage Therapy to initiate inspections of massage therapy businesses and educational programs without notice and requires massage therapy board members to complete yearly human trafficking awareness training.
House Bill 993, sponsored by Rep. Alan Powell, R-Hartwell, creates the felony offense of grooming of a minor and creates new penalties for offenses relating to visual mediums depicting minors engaged in sexually explicit conduct.
House Bill 1201, sponsored by Rep. Houston Gaines, R-Athens, allows human trafficking survivors who received first offender or conditional discharge status to vacate that status for certain crimes, as long as the crime was a direct result of being a victim of human trafficking.
Coastal communities
Earlier today in Brunswick, Kemp signed legislation impacting Georgia coastal communities, including House Bill 244, which amends the laws around how wild game can be hunted and how seafood dealers operate, and House Bill 1341, which designates white shrimp as the state’s official crustacean.
Taxes
Earlier this month Kemp signed several bills related to taxation, including House Bill 1015, sponsored by Rep. Lauren McDonald, R-Cumming, which lowers the state income tax for tax year 2024 to 5.39%, accelerating a multiyear drop in state income taxes that started at 5.75% in 2023 and will continue through 2029.
The Governor’s Office of Planning and Budget estimates the tax cut acceleration will save Georgia taxpayers approximately $1.1 billion in calendar year 2024 and about $3 billion over the next 10 years.
Kemp also signed House Bill 1021, sponsored by Rep. Lauren Daniel, R-Locust Grove, which increases the state’s income tax dependent exemption to $4,000 from $3,000.
House Bill 581, sponsored by Reps. Shaw Blackmon, R-Bonaire, and Clint Crowe, R-Jackson, enables a constitutional amendment (House Resolution 1022) to let voters decide whether counties can provide a statewide homestead valuation freeze, which limits the increase in property values to the inflation rate.
The governor has until May 7 to sign or veto bills passed during the legislative session that ended on March 28. Those he takes no action on will automatically become law.
Legislation signed by Kemp is posted on the governor’s website.
Read these related stories:
Have questions, comments or tips on education in Georgia? Contact Jill Jordan Sieder on X @journalistajill or at [email protected].
Facebook @STATEAFFAIRSGA
Instagram @STATEAFFAIRSGA
LinkedIn @STATEAFFAIRS




